
Exploring the OCD Spectrum: Understanding and Treating Various Subtypes
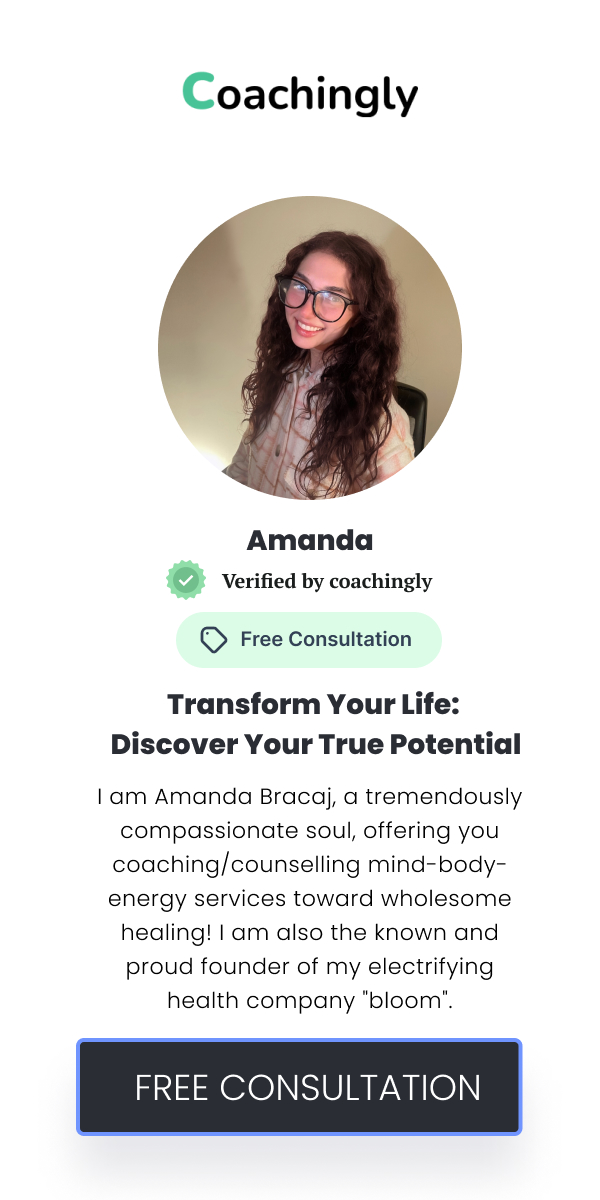
![]() Amanda Bracaj
Amanda Bracaj
![]() July 25, 2024
July 25, 2024
Obsessive-Compulsive Disorder (OCD) is a complex mental health condition characterised by persistent, intrusive thoughts (obsessions) and repetitive behaviours (compulsions). While OCD is often perceived as a single disorder, it actually encompasses a spectrum of subtypes, each presenting unique challenges and requiring tailored treatment approaches. Understanding the various subtypes of OCD is crucial for effective management and support, particularly for those affected and their loved ones. This exploration delves into the specific subtypes of OCD, the strategies for managing them, and the holistic approaches that can complement traditional treatments. Obsessive-Compulsive Disorder manifests through a range of symptoms and behaviours, impacting individuals in diverse ways. At its core, OCD involves the experience of distressing thoughts that compel individuals to engage in specific actions or mental rituals to alleviate the perceived anxiety. The spectrum of OCD reflects the varied ways these obsessions and compulsions can present themselves, from fears of contamination to the need for symmetry. This broad spectrum highlights the necessity of recognising the specific subtype one may be experiencing, as each subtype can significantly affect daily functioning and mental health. By understanding the spectrum, individuals can better identify their symptoms and seek appropriate, targeted treatment. Contamination OCD Relationship OCD Scrupulosity OCD Harm OCD Symmetry and Order OCD Checking OCD Hoarding OCD Existential OCD Effective treatment for OCD requires a comprehensive approach that addresses both the psychological and practical aspects of the disorder. Cognitive Behavioural Therapy (CBT) and Exposure and Response Prevention (ERP) are foundational techniques that help individuals confront their fears and reduce compulsive behaviours. Medications such as selective serotonin reuptake inhibitors (SSRIs) can be useful in managing symptoms, often in conjunction with therapy. Integrating holistic practices, such as mindfulness and self-compassion, can complement traditional treatments and support overall well-being. Trauma-informed care is particularly important for individuals whose OCD may be linked to past traumatic experiences. Building a robust support system, including family, friends, and peer support groups, is essential for ongoing recovery and managing OCD effectively. Creating an effective treatment plan for OCD involves a collaborative approach between individuals and their mental health professionals. Personalising the plan to address specific needs and preferences is crucial for achieving the best outcomes. Regularly assessing progress and adjusting the treatment plan as needed ensures that individuals continue to receive appropriate support. Encouraging self-care practices and building resilience are key components in managing OCD and improving overall quality of life. Setting realistic goals and celebrating small victories can foster a sense of accomplishment and motivation. By focusing on both the psychological and practical aspects of OCD, individuals can work towards a more balanced and fulfilling life. For those seeking to expand their knowledge of OCD and explore effective treatment options, several resources are available. Recommended readings include books on OCD and its treatment, as well as reputable online platforms offering information and support. Professional organisations dedicated to OCD and related disorders can provide additional resources and networking opportunities. Finding a certified life coach with expertise in OCD and trauma-informed approaches can offer personalised guidance and support. Engaging with these resources can enhance understanding and contribute to more effective management of OCD.Understanding OCD and Its Spectrum
Detailed Overview of OCD Subtypes
Contamination OCD is marked by intense fear of germs, dirt, or other forms of contamination. Individuals with this subtype may engage in excessive hand washing, cleaning, or avoidance of perceived contaminated objects. The compulsions associated with contamination OCD often stem from a profound fear of illness or disease. Addressing this subtype involves exposure and response prevention (ERP) techniques, which gradually expose individuals to feared situations while discouraging the accompanying compulsive behaviours. Cognitive Behavioural Therapy (CBT) is also beneficial in challenging and reframing the irrational beliefs underlying these fears. By targeting these specific fears, treatment can help reduce the distress and functional impairment associated with contamination OCD.
Relationship OCD revolves around persistent doubts and intrusive thoughts about one's relationship, often involving fears of not being "in love enough" or questioning the compatibility with a partner. These doubts can lead to constant seeking of reassurance, excessive analysing of the relationship, or even intrusive questioning of one's own feelings. Treatment for relationship OCD typically involves cognitive restructuring to address and challenge these doubts. ERP can also help by gradually exposing individuals to the discomfort of uncertainty without engaging in reassurance-seeking behaviours. This approach helps individuals build confidence in their own feelings and the stability of their relationships.
Scrupulosity OCD is characterised by excessive concern with moral or religious issues, often manifesting as fear of committing sins or failing to adhere to religious practices. Individuals may experience intense guilt and engage in repeated rituals to atone for perceived transgressions. Effective treatment for scrupulosity OCD involves helping individuals differentiate between genuine moral concerns and irrational fears. CBT and ERP can be employed to challenge and reduce the compulsive behaviours driven by these fears. Incorporating mindfulness and self-compassion practices can also aid in alleviating the excessive guilt associated with this subtype.
Harm OCD is characterised by intrusive thoughts about causing harm to oneself or others, despite having no intention or desire to act on these thoughts. These distressing thoughts can lead to compulsive checking or avoidance behaviours to prevent potential harm. Treatment for harm OCD often involves ERP, where individuals gradually confront these distressing thoughts without resorting to compulsions. CBT can help in reframing the intrusive thoughts and reducing the anxiety associated with them. Providing reassurance and understanding that these thoughts do not reflect one's true intentions is crucial in managing harm OCD effectively.
Individuals with symmetry and order OCD experience a compelling need for things to be arranged in a specific way or for symmetry to be maintained. This need often leads to time-consuming rituals and significant distress when things are not aligned as desired. Treatment for this subtype focuses on reducing the need for order and symmetry through gradual exposure and challenging the underlying beliefs about the necessity of these rituals. CBT and ERP can help in breaking the cycle of compulsive behaviours by encouraging tolerance of disorder and promoting flexibility. Addressing the perfectionistic tendencies that contribute to this subtype is also essential for effective treatment.
Checking OCD involves compulsive checking behaviours, such as repeatedly ensuring doors are locked or appliances are turned off, driven by fear of harm or disaster. This subtype can significantly impact daily life, causing delays and distress. Treatment often includes ERP to expose individuals to the discomfort of uncertainty and to reduce the frequency of checking behaviours. CBT helps in addressing the catastrophic thoughts that drive the checking compulsion. Strategies such as setting limits on checking behaviours and employing cognitive restructuring techniques are also effective in managing this subtype.
Hoarding OCD is characterised by difficulty discarding items, leading to clutter and distress. This subtype often involves fears of losing important information or items, leading to excessive accumulation. Treatment for hoarding OCD focuses on addressing the underlying beliefs about the significance of items and reducing the emotional distress associated with discarding them. CBT and ERP are used to help individuals confront their fears and develop strategies for organising and decluttering. Supportive interventions may also include working on decision-making skills and addressing the emotional attachments to possessions.
Existential OCD involves obsessive thoughts about existential questions, such as the meaning of life or the nature of existence. These thoughts can lead to significant anxiety and compulsive seeking of philosophical or existential answers. Treatment for existential OCD often includes CBT to help individuals challenge and reframe their obsessive thoughts. Incorporating mindfulness techniques can help individuals manage the anxiety associated with existential concerns. Encouraging engagement in meaningful activities and focusing on practical goals can also be beneficial in addressing this subtype.Approaches to Treatment and Support
Navigating the Path to Wellness
Resources for Further Learning
Recent Articles
Exploring Holistic Wellness: Integrating Mind, Body, and Energy Healing
Understanding Holistic Wellnes...
![]() Aug 05, 2024
Aug 05, 2024
The Power of Trauma-Informed Care: Transforming Lives with Compassion and Understanding
Understanding Trauma-Informed ...
![]() Aug 04, 2024
Aug 04, 2024
Navigating Mental Health Conditions: A Comprehensive Guide for Support and Healing
Understanding Mental Health Co...
![]() Aug 03, 2024
Aug 03, 2024
Understanding and Supporting Neurodivergent Individuals: Embracing Unique Perspectives
Embracing NeurodiversityNeurod...
![]() Aug 02, 2024
Aug 02, 2024
Healing from Substance Use Disorders: Compassionate Strategies for Recovery
Understanding Substance Use Di...
![]() Aug 01, 2024
Aug 01, 2024
Celebrating 2SLGBTQIA+ Identity: Creating Inclusive and Affirming Spaces
Understanding 2SLGBTQIA+ Ident...
![]() Jul 31, 2024
Jul 31, 2024
Honouring Indigenous Wisdom: Integrating Traditional Knowledge into Modern Healing Practices
In recent years, there has bee...
![]() Jul 30, 2024
Jul 30, 2024
Addressing Intersectional Discrimination: Building Empathy and Understanding in Therapy
The Complexity of Intersection...
![]() Jul 29, 2024
Jul 29, 2024
Overcoming Stigma in Schizophrenia: Effective Therapies and Support Systems
Understanding Schizophrenia an...
![]() Jul 28, 2024
Jul 28, 2024
Navigating Grief and Bereavement: Holistic Approaches to Healing from Loss
Understanding Grief and Bereav...
![]() Jul 27, 2024
Jul 27, 2024
Healing from PTSD and C-PTSD: Tailoring Therapies for Comprehensive Recovery
Understanding PTSD and C-PTSDP...
![]() Jul 26, 2024
Jul 26, 2024
ADHD and Autism Spectrum Disorders: Recognising and Supporting Diverse Needs
Understanding ADHD and Autism ...
![]() Jul 24, 2024
Jul 24, 2024
The Role of Practical Compassion in Holistic Healing: Enhancing Individual and Collective Wellbeing
Understanding Practical Compas...
![]() Jul 23, 2024
Jul 23, 2024
Understanding the Role of a Mental Health Counsellor
The True Standard of Quality H...
![]() Jul 22, 2024
Jul 22, 2024
